Detecting Parkinson's Disease with MEG
Our research demonstrates that a five minute MEG scan can accurately distinguish individuals with Parkinson's disease from healthy controls.
We’re exploring your interest in a potential crowdfunding campaign planned for early 2025. This would be aimed at our early supporters (like you) as we introduce MEG technology to those looking to better understand and manage their brain health. If you’d like more information, please let us know.
Parkinson’s disease (PD) is a progressive neurological disorder that primarily affects movement and cognition. It results from the degeneration of dopamine-producing neurons in the brain, particularly in the substantia nigra, a region critical for motor control. Symptoms include tremors, stiffness, slowed movement, and difficulties with balance, as well as non-motor symptoms such as cognitive decline and mood disorders. The exact cause of PD remains unclear, but a combination of genetic and environmental factors is thought to contribute.
Our research on PD reveals how the disease impacts the brain’s rhythms or oscillations, showing clear differences between people with PD and those without. Using MEG, we explored these alterations to identify how PD disrupts brainwave patterns and to uncover potential tools for better diagnosis. Here’s a summary of what we found.
Parkinson’s Disease: What’s Happening in the Brain?
PD is known for slowing down both movement and thinking due to changes in the brain, specifically in the areas that help control those functions. Our study zoomed in on the idea of "neural slowing" — a shift where brain waves move to lower frequencies. Using MEG, we captured these subtle shifts by studying brainwave patterns across 199 participants, including 78 with PD. With this, we could identify and separate brain patterns specific to PD.
Key Findings: What Stands Out?
1. MEG’s Unique Ability to Capture Parkinson’s Brain Changes
MEG allows for detailed observation of brain wave activity, which is particularly important in identifying changes that occur with PD. Our research found that MEG was especially sensitive to shifts in brain oscillations — specifically, the slowing down of brain waves associated with Parkinson’s. By observing these shifts, we achieved a high AUROC score (0.88), suggesting that MEG is not only effective at differentiating between PD and non-PD brains, but also highly accurate.
2. Brain Waves Tell the Story:
Posterior Slowing: For people with PD, the posterior (rear) part of the brain shows a “slowing” effect. Specifically, there’s an increase in low-frequency waves (like theta waves) and a drop in higher frequencies (like gamma waves), which helps set apart PD patterns from normal brain aging. In simpler terms, this means that the brain’s electrical activity moves towards lower frequencies, which is a common marker of neurodegeneration.
Complex Patterns Beyond Slowing: By looking deeper, we identified that PD doesn’t just involve slowing. The changes caused by PD appear evenly across both sides of the brain, providing a fuller picture of how PD changes the brain’s activity.
3. Predictive Models for PD:
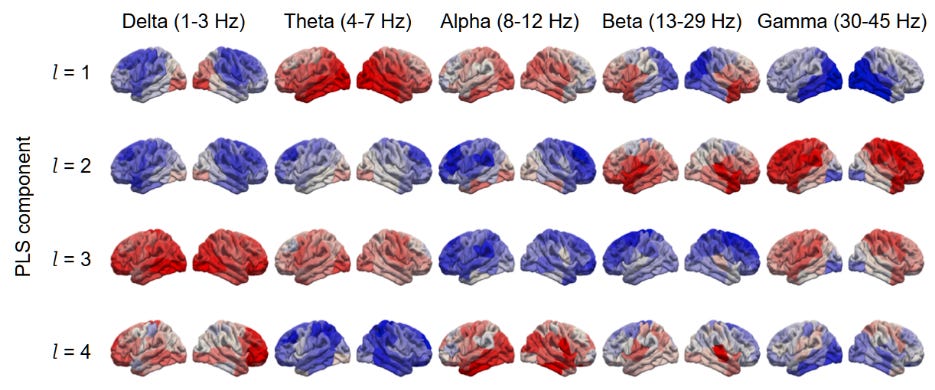
Our team built a machine learning model, which focuses on the brain’s power in specific frequency bands. The model performed best with four main “components” or features. With this setup, the MEG data effectively differentiated PD brains from healthy ones.
The image highlights brain regions where brainwave activity is either increased (red) or decreased (blue) in PD. These distinct patterns, seen across different brainwave types, help distinguish individuals with PD from those without.
What Are The Implications?
The study’s findings highlight several important implications:
Potential for Early Detection: Since MEG can capture these distinct oscillatory patterns before overt symptoms appear, it shows promise as a tool for early PD detection. Earlier diagnosis can open the door to timely interventions that may slow disease progression.
Customised Treatment Strategies: The discovery of unique brain wave patterns across different regions suggests that personalised treatment approaches targeting specific neural networks might be possible in the future.
Non-Invasive Biomarkers: The effectiveness of MEG as shown in our study suggests that non-invasive brain imaging techniques could be developed as reliable biomarkers for PD, making diagnosis easier and potentially replacing several current, more invasive methods.
Looking Ahead
By mapping out these unique oscillatory patterns in PD, our study provides a deeper understanding of how the disease affects brain function. MEG’s high sensitivity to these changes makes it a promising candidate for a clinical diagnostic tool, capable of distinguishing PD from normal brain ageing with high accuracy.
This innovative approach opens up new possibilities for early diagnosis, personalised interventions, and a more refined understanding of neurodegenerative processes in the brain.
Reference: Roberts, G., Hardy, S., Chen, R., Dunkley, B. T., PREVENT-AD Research Group, & Quebec Parkinson Network. (2024). Individual cases of Parkinson’s disease can be robustly classified by cortical oscillatory activity from magnetoencephalography. medRxiv. https://doi.org/10.1101/2024.08.27.24312669