Rewriting the Brain: A Journey to Recovery from Long COVID
A Case Study on Using MEG to Monitor Recovery After Therapeutic Interventions
We’re exploring your interest in a potential crowdfunding campaign planned for early 2025. This would be aimed at our early supporters (like you) as we introduce MEG technology to those looking to better understand and manage their brain health. If you’d like more information, please let us know.
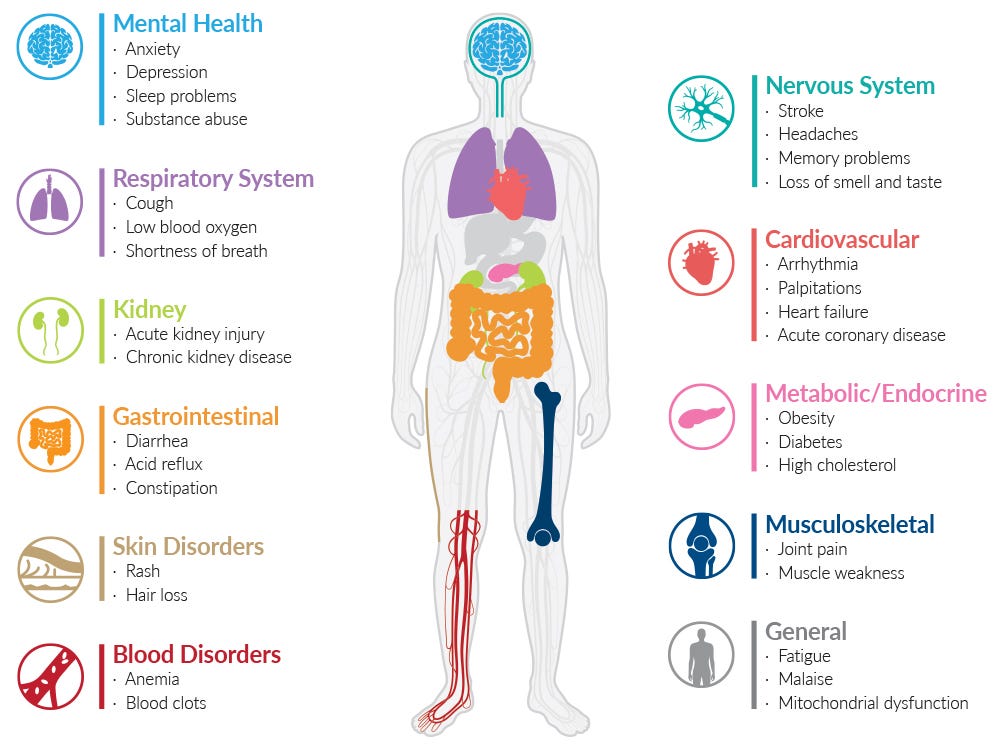
Long COVID has emerged as one of the most challenging health crises in recent years, leaving countless individuals struggling with persistent symptoms long after their initial COVID-19 infection. These symptoms - ranging from chronic fatigue and relentless brain fog to heightened anxiety and even debilitating migraines - can last for weeks, months, or longer, significantly impairing quality of life.
For many, the road to recovery is uncertain and complex.
Insights from recent studies:
Recent studies have highlighted the complexities of long COVID and its effects on the brain:
Zhao et al. (2024) revealed that even two years after recovering from COVID-19, some survivors show significant changes in brain activity, particularly in regions linked to memory, emotion, and attention - offering insight into persistent issues like mental fatigue and brain fog.
Rua et al. (2024) found long-lasting changes in the brainstem, linked to inflammation, which were more pronounced in areas controlling breathing and other vital functions. Furthermore, Wood et al. (2024) reported that those with long COVID who experience brain fog show disruptions in the blood-brain barrier and ongoing inflammation in the brain.
Serrano del Pueblo et al. (2024) and Hosp et al. (2024) found that long COVID patients experience brain changes, particularly in white matter regions, which are closely linked to impairments in episodic memory, overall cognitive function, attention, and verbal fluency.
These findings collectively highlight how long COVID affects various brain regions and mechanisms, contributing to persistent cognitive impairments and neurological symptoms.
In our case study, we explore the recovery journey of a male client, in his early thirties, who started a therapeutic program aimed at addressing the cognitive, emotional, and physiological challenges associated with Long COVID. His progress was monitored using two MEG brain scans taken over the course of several months, offering a unique insight into the brain's ability to recover.
The data revealed significant changes in brain activity, connectivity, and overall cognitive function.
Key Findings from Brain Scans
1. Functional Brain Age Improvement
At the time of the first scan, the client's functional brain age was measured at 46.9 years - far above his chronological age. By the time of the second scan, this number had reduced to 38.9 years, indicating an improvement and a shift in brain function towards his chronological age.
2. Improved Sleep Patterns
The client's initial sleep score was 14 out of 27 (using self-reported metrics), indicating poor sleep quality and a possible reliance on sleep aids. By the second scan, this score had improved to 11 out of 27, reflecting better sleep patterns and reduced reliance on medication.
3. Enhanced Concentration and Cognitive Performance
The client also demonstrated a significant boost in concentration, improving from the 29th percentile to the 69th percentile. This marked improvement aligned with self-reported gains in focus, mental clarity, and emotional regulation.
Changes in Brainwave Activity
The brain scans also revealed significant changes in brainwave activity and network connectivity:
Increased Theta Activity: Linked to improved cognitive control and working memory.
Decreased Gamma Activity: Reduced hypervigilance and mental fatigue.
Network Changes: Central Executive, Motor, and Attention networks showed enhanced connectivity, leading to improved focus, better task management, and fewer distractions. The Default Mode Network displayed decreased connectivity, correlating with reduced mental rumination and enhanced emotional regulation.
These measurable changes in brainwave activity and connectivity directly align with the client's self-reported improvements in reduced fatigue, clearer thinking, and better emotional stability.
The image displays theta activity between two scans, with darker colors indicating higher levels of theta activity. Theta waves have been reported to be markers of neuroplasticity.
A Clinically Significant Gain
The improvements observed in this case study are not just numbers on a report - they represent a measurable shift in the client's quality of life. With better sleep, sharper focus, and improved emotional well-being, the client has experienced a meaningful recovery that showcases the power of targeted therapeutic interventions.
The Role of MEG Scans in Recovery Tracking
MEG scans are a powerful, non-invasive imaging tool that measures the magnetic fields produced by brain activity. This technology provides precise temporal and spatial insights into brain function, making it especially valuable for tracking changes in brain activity, cognitive, behavioural and emotional processes.
MEG scans, as demonstrated in this case, are not only instrumental in monitoring recovery from Long COVID but also have far-reaching potential in assessing and optimizing interventions for other neurological and psychological conditions. They provide clinicians and researchers with a powerful tool to track brain function in real-time and guide effective treatment strategies.
Always consult a qualified healthcare professional before starting any treatment program.
For more information or to book a brain scan, visit www.myndspan.com.